CHIP Improves Children's Access to Care, Eases Financial Burden on Families (In Focus Brief)
CHIPRA 10-State Evaluation
Prepared for:
U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation
Key Findings:
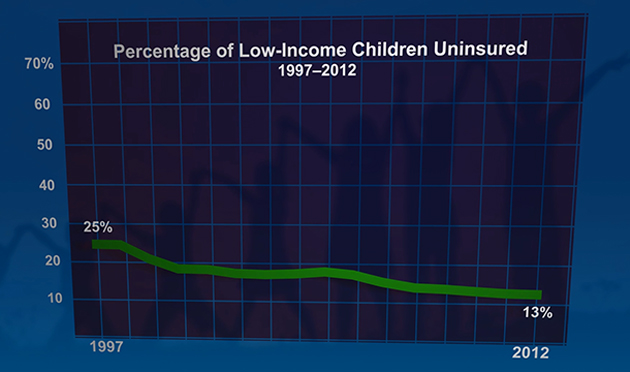
- CHIP, along with Medicaid, contributed greatly to the decline in uninsured rates among low-income children, which fell from 25 percent in 1997 to 13 percent in 2012. Since CHIP was enacted, coverage rates improved for all ethnic and income groups, and coverage disparities narrowed significantly for Hispanic children.
- Nationwide, Medicaid and CHIP participation rates increased from 82 percent in 2008 to88 percent in 2012, even as the number of eligible children has grown. Meanwhile, the number of eligible children who remain uninsured fell from 4.9 million in 2008 to 3.7 million in 2012.
- Enrollment in both Medicaid and CHIP worked as intended to provide a safety net for low-income children, especially during economic downturns. For example, the 2008 recession coincided with the largest-ever increase in CHIP enrollment.
- Most new CHIP enrollees stayed insured continuously in public coverage (Medicaid or CHIP) for more than two years, and the vast majority left because they were no longer eligible. Many children moved between Medicaid and CHIP; although most made a seamless transition, short gaps in coverage were common in some states, especially among children moving from Medicaid to CHIP.
- Children in Medicaid and CHIP had better access to care, fewer unmet needs, and greater financial protection than uninsured children. Compared with children with private insurance, CHIP enrollees had better access to dental benefits, and their families had much lower financial burden and stress in meeting the children’s health care needs.
- Most low-income families knew about Medicaid and CHIP, and those with children enrolled in the programs reported positive application experiences. However, some barriers to enrollment remain for eligible but uninsured children.
- Relatively few low-income children in CHIP have access to private insurance coverage; the rate of children directly switching from private to public coverage at the time of CHIP enrollment was as low as 4 percent. Even when dependent coverage is available to families with children in CHIP, affordability is likely a barrier many parents face in obtaining employer-sponsored coverage for their children.
A nationwide evaluation of the Children’s Health Insurance Program (CHIP) reveals that CHIP has successfully expanded health insurance coverage to children who would otherwise be uninsured, thereby increasing their access to health care and reducing the financial burden on their families. Mandated as part of the Children’s Health Insurance Reauthorization Act (CHIPRA) of 2009, this evaluation presents new information on the evolution of CHIP from 1997 to 2012, including whether the program is meeting its goals and how it was affected by CHIPRA and the Affordable Care Act.
How do you apply evidence?
Take our quick four-question survey to help us curate evidence and insights that serve you.
Take our survey
